In 2021, we were already seeing important disruptions in how key stakeholders engage one another. The momentum will build in 2022. We’re watching new roles grow while long-trusted roles change; new channels open and others open even wider.
For this trend, we'll look at the changing interface through five key lenses:
1. HCPs to biopharma: the growth of the hybrid field force
2. Sponsors to sites: a changed future for CRAs
3. HCPs to sites: the new path to recruitment acceleration
4. HCPs to consumers: the rise of the physician influencer
5. Patients to products: an ever more powerful search for a treatment
One of the biggest commercial changes we’ve seen over the last 12 months is the integration of field roles.
Nurse educators, reimbursement specialists, field reps and engagement center representatives have all been integrated through CRM, through technology. That’s enabled them to work together and embrace each other's responsibilities and areas of expertise, ultimately making sure that value is brought across the platform of commercial.
For the healthcare professional that growing integration streamlines how many people are interacting with the provider office. For the biopharma company, it cross-trains talent on different aspects of the complex ecosystem our healthcare stakeholders are working in.
The field rep takes something of an orchestrator role in this changing model, being a key point in understanding what an account needs at a particular moment, whether that’s the convenience of an engagement center, depth of a reimbursement expert, speed of a quick email or high service of a nurse educator. As each interacts with the practice—virtually or in person—they bring along a bit of each of the other roles.
The need to work effectively in these new hybrid models has changed how some leaders think about hiring. Instead of focusing on category expertise or success in previous isolated roles, they’re talking about competencies like continuous learning, managing a territory, understanding marketing, embracing different triggers.
Those competencies show the ability to understand and act in a local ecosystem, but they can also be even more targeted than that. In this hybrid environment, working across channels and teams, the right competencies ensure that reps know how to observe and evaluate what a physician or office may need that might be different than the office that's just down the road.
In the next three years the role of clinical research associate (CRA) will change significantly, evolving from working nearly 100% on source data verification to increasingly being a critical resource for risk-based monitoring.
Like so many other shifts, this one was certainly sped along by COVID-19. When CRAs could no longer visit sites to collect data, they had to quickly pivot to using digital platforms to collect and evaluate data. With less on-site data collection, CRAs were freed to support other initiatives around quality and performance at the sites.
While CRAs may still perform site visits, the frequency of those visits is expected to continue decreasing, allowing them to work in more flexible environments and at the top of the skillsets. The CRA of 2022 or 2023 might expect to work more like a data analyst, evaluating enrollment against protocol, reviewing drug accountability and verifying adverse events.
They will increasingly be focused on critical study risks and overall site performance.
Geographically freeing CRAs will open up new conversations about increasingly centralizing core functions while decentralizing the patient trial experience.
The greatest challenge to completing clinical trials on time is recruitment.
Competition for patients is intense. Delays are costly when study recruitment and enrollment are not completed on time or when sites do not meet their recruitment numbers, sometimes putting the study itself in jeopardy. Today, 50% of trials are extended due to poor recruitment performance. Meanwhile, our sites are investing almost one third of their time on recruitment activities.
In 2022, sponsors will increasingly take on the twin challenges of accelerating recruitment and reducing burden on the sites. Today, most recruitment plans rely on two strategies: (1) tools to enable that site activity and (2) direct-to-patient advertising. What’s missing? The doctors who patients turn to for their everyday healthcare and advice for advances in care. A third way is set to accelerate recruitment in 2022: increasing awareness and education about a trial amongst physicians treating relevant patients near the sites.
Because of their personal relationship with patients, healthcare professionals can play a powerful role in the referral process, providing information and reassurance that help to raise awareness, trust and motivation to enroll.
According to the National Institutes of Health, 77% of patients who participate in a clinical trial learned about the trial from their healthcare professional. When asked, most healthcare professionals say they are eager for their patients to participate in clinical trials. Yet, they are busy with the daily concerns of their work with patients and far too often lack awareness of ongoing studies, including those within reach of their offices, that could potentially benefit the patients currently in their practices. Historically, potential referring healthcare professionals proactively would need to go to a digital destination to find out more about active clinical trials—and with a lack of awareness of where to go, and a lack of time even when they know where to go, referrals are often de-prioritized, particularly in noncritical care situations.
Now, however, advances in precision targeting, synchronized experiences and performance analytics are making it possible to locate the right healthcare professionals in the right locations and drive awareness and interest through relevant messaging.
In 2022, sponsors will be able to engage trusted healthcare professionals, treating hundreds or thousands of relevant patients, at the individual level. These approaches have three specific benefits: improving awareness among trusted advisors, increasing awareness about the trial design and ultimately fueling conversations between patients and their healthcare professionals.
“Because of their personal relationship with patients, healthcare professionals can play a powerful role in the referral process, providing information and reassurance that help to raise awareness, trust and motivation to enroll.”
Learn more about the advances Syneos Health is taking to improve Clinical Trial Recruitment and Retention
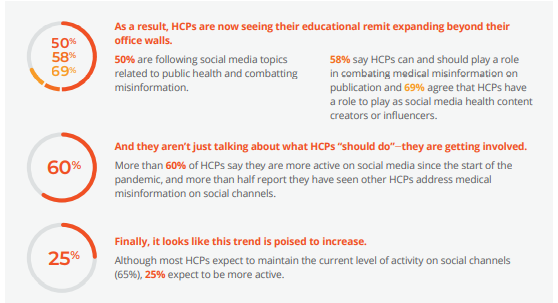
We’ve all heard about the problematic side of social media. Now, we are starting to learn how healthcare professionals (HCPs) see it. For HCPs, social media isn’t just a theoretical problem, according to a recent survey. They are most concerned about people challenging evidence-based medical advice based on bad information.
- HCPs more than passive consumers of social media content
- More than half of HCPs are sharing some form of information they see on social media
- One-third are responding or engaging with colleagues’ social media content
- Nearly 20% are posting their own video or other content
The destination for first-level care is changing in the US. Pharmacy chains, big box stores and telehealth outlets are increasingly standing in for traditional office-based care. Many of the new channels have two things in common set to dramatically change both preventative and acute care:
- Menu-based healthcare ordering
- Retail pricing
Via a menu of choices, consumers can select just the services they want to focus on, whether that’s addressing a chronic condition or refilling an existing medication. The pricing for these services is most often a flat fee, one that can be covered by insurance but is often affordable for the underinsured.
Consumers are shopping for the care they want to prioritize, essentially self-diagnosing and self-selecting before even entering the healthcare marketplace.
There’s no better example of this phenomenon than menu-based online telehealth. With the search of a symptom, users can quickly find their way to a complete medical service list. Choose from anything from urinary tract infection to acne treatment to acid reflux and within minutes connect with a prescriber via text who will remotely diagnose and send a prescription.
In the coming years, doctors will need to work hard to stay connected to their patients and encourage them to think of their whole health, not just the pressing symptom of the moment.
Biopharma companies and HCPs should also keep a close eye on payer-led initiatives . In 2022, insurers and hybrid payer/provider entities (“payviders”) will innovate aggressively in this space using tools of eHealth and telemedicine that were perfected during the COVID-19 pandemic. An example is NavigateNOW, a cost-conscious, $0-copay health plan launched by UnitedHealthcare’s Optum unit.13
Leveraging a network of more than 50,000 doctors UHC/ Optum brought in-house by acquiring physician practices, NavigateNOW will create virtual care teams customized to the patient’s needs and the first point of care will be on a screen, with in-person visits scheduled as necessary. Competition from Amazon, Apple and a host of technology startups may be driving this trend, but "payviders" bring significant resources—not least, controlling formularies and holding the purse strings.
Get the printable PDF of Trend #4: The Changing Customer Interface, here. Or, subscribe now to access the full 2022 Health Trends report and our monthly email to receive exclusive updates.